Managing the Flare-Up
Managing the Flare-Up: A Holistic Toolkit for Challenging Pain or Fatigue Days

“Your Health Is in Your Hands.” - Nature's Pure Love Ltd
Periods of heightened pain or exhaustion, often called
flare-ups, can feel like waves that take over daily life. For many living with
chronic pain, fatigue, or other long-term Dis-Ease, these days are part of a natural rhythm. Though difficult, they do not always mean the underlying condition has worsened. Rather, they signal that the body is calling for deeper rest, gentle care, and intentional balance.
This guide offers a holistic framework for navigating flare-ups — supporting body, mind, and spirit through proactive preparation, energy management, comfort measures, and emotional stabilisation. It draws on evidence-based approaches and self-care strategies from leading wellness and medical resources to help you maintain stability even when Dis-Ease flares.
1. Understanding the Flare Dynamic and Reframing the Experience
A flare-up is a period in which symptoms such as pain, fatigue, or brain fog increase significantly, often making daily routines challenging. It is essential to remember that flare-ups are temporary phases, not signs of permanent decline.
According to the Agency for Clinical Innovation (ACI), reframing flares as temporary challenges rather than crises of worsening health is the first step towards regaining calm and control. View a flare as communication, not catastrophe — the body is signalling a need for recalibration, rest, or decompression.
2. Proactive Preparation: Recognising Triggers and Patterns
Preparation is the cornerstone of flare-up management. The Arthritis Foundation recommends identifying red-flag triggers (activities, foods, stressors, or emotions that aggravate symptoms) and green-flag actions (supportive behaviours that promote balance).
Triggers may include:
- Overexertion or underactivity
- Emotional strain or low mood
- Poor sleep or skipped meals
- Environmental changes such as heat, cold, or sensory overload
Because chronic pain and fatigue are closely linked to the central nervous system, managing stress and stabilising mood are direct preventative measures (PTCOA, n.d.). Keeping a reflective journal or activity diary helps identify trends — for example, whether certain events or emotions precede symptom increases (CFS Self-Help, n.d.).
3. Creating a Personal Flare-Up Action Plan (FAP)
During difficult days, clear guidance can prevent panic. A Flare-Up Action Plan (FAP) serves as a structured roadmap outlining what to do when symptoms intensify (VA.gov, n.d.). Review it with your healthcare professional so it complements your care approach.
Include:
- Physical comfort tools: heat pads, warm baths, or gentle stretching.
- Cognitive reminders: written affirmations such as “This will pass.”
- Behavioural adjustments: scaling back activities but avoiding total rest.
The International Association for the Study of Pain (IASP) emphasises that some movement is better than none — complete inactivity can reinforce avoidance patterns. The goal is to titrate activity, balancing flexibility with gentle motion.
4. Conserving Energy: The Art of Pacing
A. The Energy Envelope Principle
For conditions involving chronic fatigue, pacing is a protective strategy. The Energy Envelope Theory suggests that functioning can be sustained only when energy use remains within personal limits, reducing the risk of post-exertional malaise.
B. The Three P’s Principle
The Three P’s — Prioritise, Plan, and Pace — provide a practical rhythm for conserving energy:
- Prioritise: Focus on essentials.
- Plan: Spread demanding tasks across the week.
- Pace: Rest before fatigue sets in, not after.
C. Communicating Limits: The Spoon Theory
The
Spoon Theory offers a simple metaphor for limited energy: each “spoon” represents a unit of capacity. On flare days, you have fewer spoons, and each task costs more (GoodRx, 2022;Burning Nights CRPS, 2021).
D. Monitoring with Body Awareness
Some people use
heart-rate monitoring to stay below the point that triggers exhaustion, known as the ventilatory or anaerobic threshold (Workwell Foundation, n.d.). This makes pacing objective, not just intuitive.
5. Physical Comfort and Gentle Movement
A. Movement During a Flare
Gentle, low-impact activity supports circulation and flexibility. Recommended stretches include (Abbott, 2020;Mayo Clinic, 2022):
- Knee-to-Chest Stretch
- Lower Back Twist
- Seated Chair Stretch
- Cat/Cow Modification
B. Heat, Topicals, and Natural Support
Warm baths, hot compresses, or heat pads can ease tension. Natural supports include:
- Turmeric (Curcumin): helps the body’s natural inflammatory response.
- Willow Bark (Salix alba): traditionally used to ease stiffness and discomfort.
Always consult a healthcare provider before starting new supplements.
6. Calming the Mind: Psychological and Emotional Stability
Pain and fatigue activate stress pathways in the brain. Calming these responses can lessen symptom intensity.
A. Cognitive Restructuring
Cognitive Restructuring (CR) helps identify and reframe unhelpful thoughts (FibroGuide, n.d.). Replace
“I can’t cope” with
“This flare is temporary.” Such language helps “close the pain gate”.
B. Mantras for Difficult Moments
Grounding phrases create reassurance (Bezzy MS, 2021):
- “This is temporary.”
- “I am safe.”
- “I’m taking care of myself.”
C. Mindfulness and Sensory Anchoring
Observing sensations without judgment reduces catastrophising. Practices such as body-scan meditation or walking meditation help bring attention to the present moment.
D. Controlled Breathing
Breathing techniques calm the nervous system:
- Diaphragmatic Breathing
- 4-7-8 Technique: Inhale 4 sec – hold 7 – exhale 8 (BHF, n.d.).
7. Hydration and Nutritional Support
A. Replenishing Fluids and Electrolytes
Electrolyte imbalance can intensify fatigue. Some people with chronic fatigue have altered blood volume or hydration (Buoy, 2023). Consistent fluid intake and balanced electrolytes support clarity and endurance
B. Nourishing Through Digestibility
When digestion is sensitive, focus on gentle foods — cooked vegetables, soft proteins, and smooth nut butters.
C. Returning to Anti-Inflammatory Choices
As symptoms ease:
- Add omega-3 foods like flaxseed or salmon.
- Limit processed oils high in omega-6 (Johns Hopkins Medicine, 2023).
- Choose whole grains and starchy vegetables
- Balance meals with lean protein and healthy fats.
8. Adaptive Living: Systems That Save Energy
A. Energy-Saving Habits
Modify routines to conserve energy:
- Sit for grooming or cooking.
- Use long-handled tools.
- Delegate heavier tasks.
B. Organisation for Clarity
Cognitive fatigue requires structure. Strategies include assigning a “home” for items, breaking projects into smaller steps, and using digital reminders or
journaling.
C. Assistive and Adaptive Tools
Energy-saving devices are acts of self-care. Examples: electric jar openers, slow cookers, shower seats, or grab bars (Chronius Health, 2023;Johns Hopkins Medicine, n.d.).
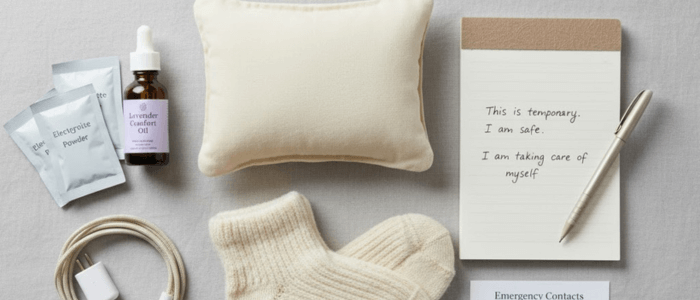
9. Building Your Flare-Up Crisis Kit
Preparedness restores confidence. A
Crisis Kit or “Go-Bag” keeps essentials ready (CPS Foundation, n.d.).
Include:
- Comfort: heat pads, soft clothing, blanket.
- Care: prescribed medications, wipes, sanitiser.
- Nutrition: electrolyte sachets, snacks.
- Connection: emergency contacts and chargers.
10. Review, Reflect, Refine
Chronic Dis-Ease management is not a linear path; it is an ongoing process of self-mastery. The period
after a flare-up is as important as the flare itself.
- The Learning Loop: Immediately after recovery, engage in structured reflection: Which behavioural adjustment in my FAP worked best? Which trigger was most prominent? These insights are valuable data points. They allow you to refine your Flare-Up Action Plan and update your Personalised Wellness Plan for future resilience, ensuring you are always evolving and strengthening your toolkit for long-term transformation.
Remember that all observations can be stored in your Journal or your pain diary
Conclusion: Preparation Is Power
A holistic response to flare-ups integrates body, mind, and environment.
Key reminders:
- Pacing is protection — use the Three P’s to balance activity and rest.
- Psychological stability modulates pain — breathing and mindfulness soothe the nervous system.
- Adaptive living saves energy — systems and tools simplify recovery.
- Nutrition and hydration support restoration.
- Preparation is power — a written plan and kit reduce stress and promote calm.
Every act of preparation tells your body: “I am listening. I am safe. I am healing.”
Discover the C.R.E.A.M. Holistic Health Plan
When you’re ready to explore structured wellness practices for long-term balance, Nature’s Pure Love invites you to learn about the C.R.E.A.M. Holistic Health Plan — a lifestyle approach designed to help you Cleanse, Restore, Energise, Align, and Maintain your natural wellbeing.
Because at NPL, we believe:
“Your Health Is in Your Hands.”
Frequently Asked Questions (FAQ)
Q: What exactly is a 'flare-up' and what does it mean for my chronic condition?
A flare-up is a temporary period where symptoms such as chronic pain, fatigue, or brain fog significantly increase, making daily routines challenging.
It is crucial to remember that a flare is not a sign of permanent decline.
We encourage you to reframe it as communication—your body is simply signalling a need for deeper rest, care, and internal recalibration, as noted by the Agency for Clinical Innovation (ACI).
Q: How does my mental state affect my pain levels during a flare-up?
Pain and fatigue activate stress pathways in the brain. Calming your mind can directly lessen symptom intensity.
Techniques like Cognitive Restructuring help you identify unhelpful thoughts (e.g., "I can't cope") and replace them with empowering ones (e.g., "This flare is temporary"), which helps to soothe the nervous system and 'close the pain gate'.
Q: How can I prepare for a flare-up before it even happens?
Preparation is the cornerstone of effective management.
Start by identifying your personal red-flag triggers (e.g., overexertion, emotional strain, or poor sleep) and keeping a reflective journal or activity diary to spot your individual patterns.
This self-awareness allows you to take preventative action.
Q: What should I include in my personal Flare-Up Action Plan (FAP)?
Your FAP should be a structured roadmap to guide you on difficult days and prevent panic.
Key components include:
Physical Comfort Tools: Heat pads, warm baths, or topical natural supports.
Cognitive Reminders: Written affirmations, such as “This will pass.”
Behavioural Adjustments: Clear guidance on scaling back activities while avoiding complete rest.
We recommend reviewing this plan with your healthcare professional.
Q: What is 'pacing' and how do the Three P’s help manage my energy?
Pacing is a protective strategy for conserving limited energy (often illustrated by the Spoon Theory). It is essential for managing chronic fatigue.
The practical rhythm is based on the Three P’s:
Prioritise: Focus only on essentials.
Plan: Spread demanding tasks across the week.
Pace: Rest before exhaustion sets in, not just when you hit your limit.
Q: Are there any natural supplements or remedies that can help manage discomfort?
Natural supports can complement your care approach.
For example, Turmeric (Curcumin) can assist the body’s natural inflammatory response, and Willow Bark (Salix alba) is traditionally used to ease stiffness.
It is essential to consult with your healthcare provider before starting any new supplements or herbal remedies.











